Freehold (732) 294-9393
Freehold (732) 294-9393

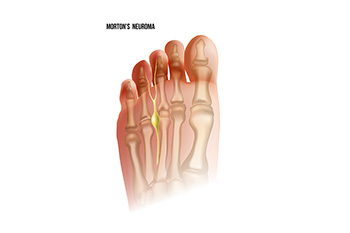
Foot pain is a common ailment. It can happen in different areas of the foot and for various reasons. Pain that occurs between the third and fourth toes may indicate Morton’s neuroma has developed. It is a condition that affects the nerve between these toes and causes it to become compressed and irritated. Morton’s neuroma is generally caused by wearing shoes that do not have enough room in the toe area, such as high heels. It is beneficial to choose a shoe with a wider toe box if high heels are desired to be worn. Common symptoms that are associated with Morton’s neuroma can consist of a burning or tingling sensation, and many people feel as if there is a small pebble in their shoe or sock. Relief may be found in the beginning stages of Morton’s neuroma by wearing shoes that fit correctly. For progressed cases, it may be necessary for a more invasive treatment to be performed. If you have pain in this part of your foot, it is suggested that you seek the counsel of a podiatrist who can effectively diagnose and offer correct treatment options for Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Henry Miller of New Jersey. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Freehold, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.

Adults who have flat feet may experience pain. It can happen occasionally or constantly, and often requires shoes that are worn to have adequate arch support. The majority of babies are born with flat feet, and an abnormal foot structure may cause the feet to remain that way through adulthood. Flat feet may also develop in people who become overweight, as a result of the added pressure the feet endure. Additionally, existing medical conditions such as diabetes, and rheumatoid arthritis may lead to getting flat feet, and it may also happen to people as the aging process occurs. The possibility of spraining or fracturing the ankle may increase as the ankle rolls inward while walking, often causing the gait to change. Many patients find relief when specific stretches are performed that target strengthening the arch, and wearing orthotics may help to diminish any discomfort from having flat feet. If you have this foot condition, it is strongly suggested that you are under the care of a podiatrist who can offer you relief options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Henry Miller from New Jersey. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Freehold, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.

Plantar fasciitis, an inflammation of the tissue that runs along the bottom of the foot, is one of the most common sources of foot and heel pain. One symptom of this condition is feeling pain after a period of rest, such as sleeping or a long car ride. Pain in the arch of the foot, swollen heels, and persistent heel pain are other symptoms. About 80 percent of people who have plantar fasciitis can also experience tightness in the Achilles tendon at the back of the heel. Furthermore, plantar fasciitis may affect the toes, ankles, and calf muscles, but these symptoms can be indirect results of the inflammation of the plantar fascia ligament. Active men and women between the ages of 40 and 70 are more at risk of developing plantar fasciitis. Taking certain medications, performing stretching exercises, and making changes to activity levels are believed to be helpful in relieving the pain of plantar fasciitis. If you need help with managing this condition, it is suggested that you make an appointment with a podiatrist for a diagnosis and appropriate treatment options.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Henry Miller from New Jersey. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Freehold, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.

Both running and walking can be beneficial to your health. Running is an aerobic activity that assists with strengthening muscles and bones, in addition to improving heart function. Walking engages the legs and core while helping to alleviate stress, enhancing cardiovascular health and overall fitness. Whether you walk or run, you may want to consider getting athletic shoes that match the activity. Doing so can ensure a more efficient workout and lessen injuries. The shoes for these two activities are different because of the various ways the feet strike the ground and the amount of force sustained by the feet. While running, you may have both feet off the ground at once, while when walking, one foot is always on the ground. Both exercisers land on their heels first, but walkers roll forward onto their toes immediately. Runners distribute more body weight across their feet than walkers. Shoes for running and walking are made to manage these different movements. If you enjoy walking or running and want to make sure your shoes are serving you well, it is suggested that you consult with a podiatrist.
For more information about walking shoes versus running shoes, consult with Dr. Henry Miller from New Jersey. Our doctor can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our office located in Freehold, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Both running and walking are great exercises, but should a person wear the same shoes for both activities? The answer is no, because there is a difference between the way a person’s feet hit the ground when they are walking and when they are running. Therefore, the shoes for each activity are designed differently. Before you begin any exercise program it is always recommended that you speak with your doctor or podiatrist.
Walking is a low impact exercise that is often recommended by doctors to their patients. While walking is a simple activity, it still requires some degree of preparation. If you think about walking and how your feet strike the ground as you move, you will notice that your heel hits the ground first before your foot continues to roll forward and your next step begins. Because of this rolling motion, walking shoes are designed to be more flexible than running shoes. This flexibility helps the walker push off with each step taken.
Because the heel hits the ground first when you walk, walking shoes are designed to absorb most of the shock. Walking shoes should therefore have a beveled or angled heel. The angle of the heel helps absorb the shock and reduces pressure from the ankles. This is especially important for speed walkers, as their feet will hit the ground twice as often as the normal walker.
When people decide to run as a hobby or for their health, they must first realize that running is a high impact exercise. If not done with the proper equipment, running may cause damage to the feet and legs. Running shoes are designed to be more lightweight and to have thicker soles. The thicker soles act as shock absorbers for the rest of the body. Walking shoes often do not have the proper arch support that running shoes do.
A proper fitting shoe can make or break a runner or a walker. If the shoes are too big, their feet will slide back and forth inside the shoe and cause blisters. Whether you will be running or walking, the right equipment can make all of the difference in the world.

We learn to walk at an early age, putting one foot in front of the other to get somewhere else. Unless you are on a trail or other uneven surface, most people have a smooth and even gait. When this normal pattern changes and the walking is less steady, it may be a sign of a problem termed ataxic gait. Symptoms include dizziness or vertigo, shuffling, loss of balance, and stumbling. Among the causes of an unsteady gait are cardiovascular disease, musculoskeletal or neurological disorders, infections, or certain medications. Someone with an unsteady gait may exhibit changes, such as standing or walking with the feet wider apart, walking more slowly, or falling more often. If you notice such changes in behavior around walking, it is suggested that you make an appointment with a podiatrist for a gait evaluation. You may be asked to walk toe to heel, and your stance, step length, and balance will be noted. At that point, the podiatrist can recommend the proper course of action for you to take to address the problem of an unsteady gait.
If you have any concerns about your feet, contact Dr. Henry Miller from New Jersey. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Freehold, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.